by Helen Smallwood, Shaftesbury Clinic
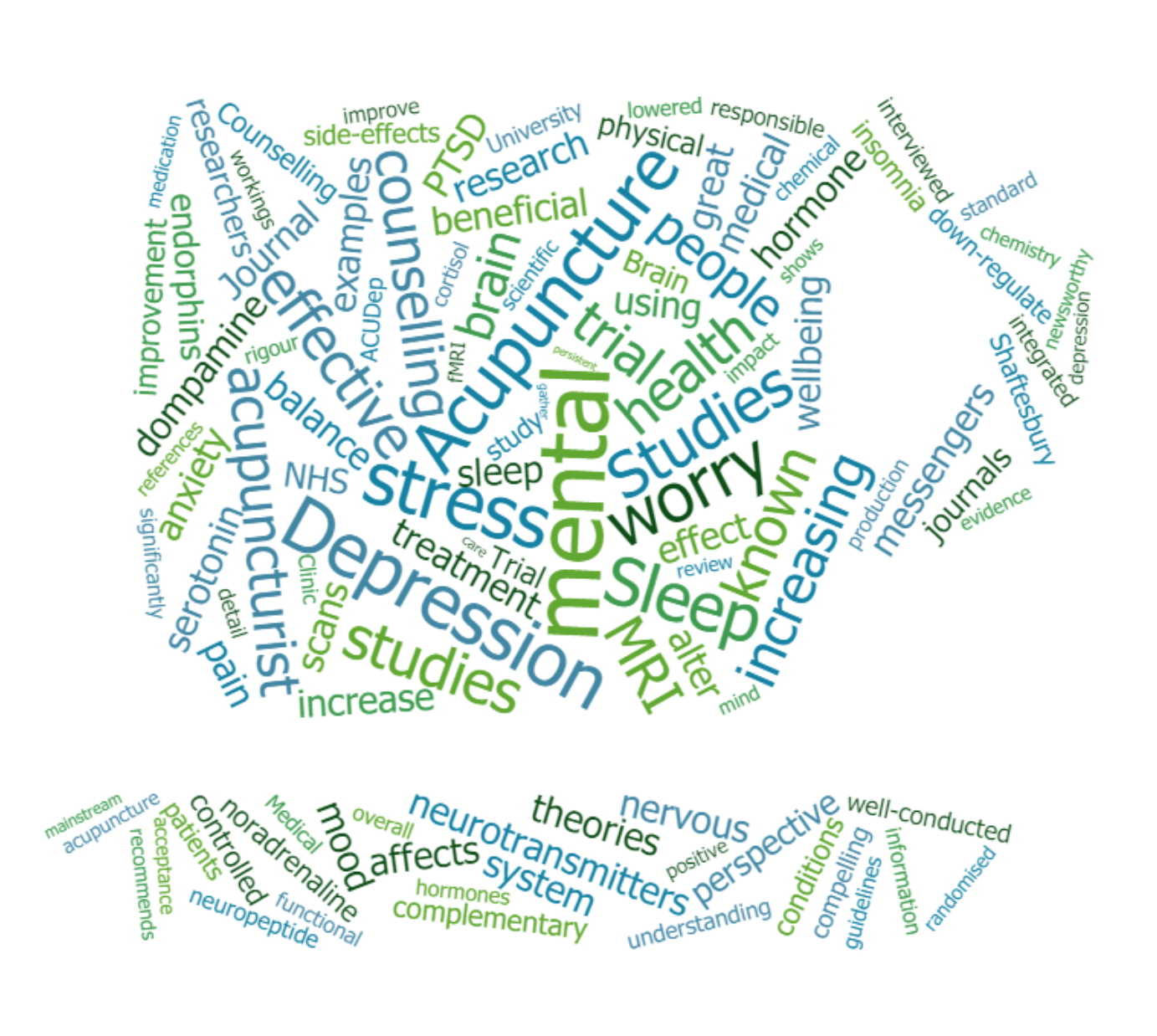
This blog post will concentrate on the use and research regarding acupuncture and mental health, and with a particular focus on depression.
Important to know: Chronic health conditions should be addressed under direct medical supervision of your GP or consultant, and acupuncture would be an adjunct or complement to usual care – we advise that you let you doctor know when you use this approach.
Acupuncture is known by many as being holistic, which means it looks at the workings of the body and the mind overall in an integrated way, as opposed to seeing them as separate entities. Some people are surprised to the extent to which acupuncture has been used and researched for mental health as their first impression is that acupuncture is a very physical therapy and they are mainly associating it with its uses for pain and injuries.
On a research database search, “acupuncture” + “mental health” yields over 48,000 hits of academic articles, 5,600 of which are “RCT”‘s (Randomised Controlled Trials) which are a high standard of research comparing acupuncture to another procedure, an inert control or “sham acupuncture” intervention. Finding that of these 5,600 studies, 43% have been carried out since 2017 shows that wide and increasing scientific research is ongoing in this area.

Acupuncture for depression came into the media’s attention recently in a three-armed trial gave very good results for acupuncture in this field (MacPherson et al, 2012). A large, study, it recruited patients from GP practises who had been diagnosed with depression in the previous 5 years.
I was asked to be interviewed for local radio regarding this study, the news coverage and acupuncture and mental health. You can listen to the interview here.
Media interest
There was a great deal of research into acupuncture and depression, following the “Acupuncture, Counselling or Usual care for Depression (ACUDep) Trial” at York University (MacPherson et al, 2012). This was a large trial (755 patients) over three years. They were allocated randomly to a) 12 weekly acupuncture sessions, b) 12 weekly counselling sessions (a and b were in addition to usual GP care), or c) usual GP care only. The researchers found that both acupuncture and counselling significantly reduced depression at 3 months when compared to usual care alone. This suggests acupuncture is an effective adjust to usual care for depression. This was a well-run trial, (a randomised controlled trial which is the gold standard of medical research). This was also commented on in the British Medical Journal (BMJ): “Adding acupuncture or counselling to usual care hastens improvement in persistent depression” (ref: Torjesen I. BMJ. 2013 Sep 25; 347:f5789. Epub 2013 Sep 25.)
In follow-up to the ACUDEP trial, Spackman et al (2014) examined the cost-effectiveness of the interventions used. Noting that depression ranked 4th in cost of disease burden in high-income nations, they saw the need for treatments that offered value for money. The QALY is the measure of cost-benefit in the NHS with £20,000-£30,000 the usual threshold for a “quality-adjusted life year”, or year in perfect health of an individual after an intervention. On these terms, acupuncture was found cost-effective in addressing depression in the research group as compared with counselling or usual care alone.
Acupuncture Background and Scientific Understanding
The theories behind acupuncture that most people are aware of, are the ancient Eastern philosophies of energy and balance, whereby acupuncture originated in China, and was also developed in Japan, Korea and other neighbouring countries, and gradually spread around the globe.
Acceptance by medical authorities: there is increasing understanding of acupuncture from the Western Medical perspective, with a great deal of scientific research being carried out, and the rigour of the research is increasing all the time. For some particular conditions the NHS now recommends acupuncture in the NICE guidelines, which shows increasing mainstream acceptance.
Brain Effects Seen in Scans – Mechanisms of Action

There have been a lot of studies looking at how acupuncture affects the brain, using functional MRI scans, and also on how it affects hormones and neurotransmitters in the blood and nervous system. Acupuncture is clearly shown to alter and balance these systems in repeated scientific studies, including animal and physiological studies of biomarkers.
All About Neurotransmitters – our chemical messengers for mood
The theories around acupuncture for depression come from research showing acupuncture can alter brain chemistry and increase serotonin production (which is lowered in depression), and acupuncture is also known to increase endorphins (the body’s feel-good hormones) in the nervous system and brain, which may improve mood.
It’s also thought that acupuncture’s effect on other chemical messengers like dompamine, noradrenaline, neuropeptide and cortisol (the stress hormone) may also come into play. In particular, it is known that acupuncture can lower cortisol (the stress hormone) which. Acupuncture has been shown to down-regulate the areas of the brain responsible for pain, stress, anxiety and worry in studies.
Sleep like a baby?
There is also some evidence on acupuncture for sleep and insomnia, which can have a large impact on mental wellbeing. As acupuncture is complementary, it can be combined with other treatment and medication, there are no side-effects and it is a very safe and minimal form of treatment.
More news
Other newsworthy pieces have come to light recently, including how the US Army is using acupuncture for veterans returning home with PTSD and brain injuries, to a very good effect PTSD in Veterans – Acupuncture research
Talk to us
Don’t forget, we are always happy to talk to you about what we do, and to answer your questions. By phone, email or in person, you can book a call-back or free 20 minute consultation to find out us and our clinic, and whether acupuncture is for you.
Links, references and resources:
British Acupuncture Council on Acupuncture and Depression: BAcC Factsheet Depression
MacPherson, H., Vickers, A., Bland, M., Torgerson, D., Corbett, M., Spackman, E., Saramago, P., Woods, B., Weatherly, H., Sculpher, M. and Manca, A., 2017. Acupuncture, Counselling or Usual Care for Depression (ACUDep): a randomised controlled trial. In Acupuncture for chronic pain and depression in primary care: a programme of research. NIHR Journals Library.
MacPherson, H., Richmond, S., Bland, J.M., Lansdown, H., Hopton, A., Kang’ombe, A., Morley, S., Perren, S., Spackman, E., Spilsbury, K. and Torgerson, D., 2012. Acupuncture, Counseling, and Usual care for Depression (ACUDep): study protocol for a randomized controlled trial. Trials, 13(1), pp.1-7.
Spackman, E., Richmond, S., Sculpher, M., Bland, M., Brealey, S., Gabe, R., Hopton, A., Keding, A., Lansdown, H., Perren, S. and Torgerson, D., 2014. Cost-effectiveness analysis of acupuncture, counselling and usual care in treating patients with depression: the results of the ACUDep trial. PloS one, 9(11), p.e113726.
Xu, Z. R. Sun, L. P. Li, Effects of acupuncture on the hypothalamuspituitary-adrenal axis in the patient of depression. Chinese Acupuncture & Moxibustion. 2004;24:78-80.
W. Sun, L. Wang, Influence of acupuncture on HPAA in a rat model of chronic stress-induced depression. Shanghai Journal of Acupuncture and Moxibustion. 2007;26:32-34